What’s the secret to surgically removing cost from a Mental Health Trust without compromising quality?
The annual budget setting cycle is often seen by NHS services as an opportunity to ask for more not less. With funding restricted NHS Trusts must work with a very different mindset.
The Finance Director can get the red pen out to seek to control spend but this approach is not sufficient to sustainably balance the books.
The secret is operationally-led financial improvement.
Read More
The answer isn’t more
Good operations look after the money, it is in the frontline that the vast majority of spend occurs and this is mostly people costs.
All mental health trusts have rapidly increased workforce in recent years. They are typically one of the biggest local employers. You will be surprised then what a small proportion of clinical staff time is spent on direct patient care.
We often run exercises across teams to get staff to detail how time is spent to identify prime opportunities for improvement. By way of example, a home treatment team’s nurses might average 25% at best directly supporting patients face to face or on the phone. The majority is consumed by administration and travel.
Ok, so some administration and travel time is reasonable, but the issue is that staff across the many mental health trusts we’ve worked with don’t know what good looks like; nor are there strong performance controls in place to drive behaviour.
In our home treatment example, staff were only with a patient mid-morning & mid-afternoon as they started and finished at base to plan for the day and access computers to write up notes.
This is a very inefficient use of time, staff recognised that a more modern approach would be to work peripatetically remotely enabled by technology to much increase the ability to see more patients. We were able to increase direct care time by a third.
So, extrapolate this across a Trust. Anyone will tell you how difficult it is to recruit more mental health staff, have you first released the huge gain by using what you’ve got already via a focus on operational rigours?
Community services
PROM measures are still immature and not yet central to decision making. When they are available they can show that the service has not made a significant difference to wellbeing.
Only talking therapies has established recovery targets and linked package of care clarity. This means a mental health trust will have hundreds of staff in community teams that have grown rapidly but not on a firm efficacy and efficiency foundation.
Efficacy measures are absent like step-down recovery rate and trusts are normally poor at combining activity with the workforce that delivered it to understand value for money measures like cost per case.
The focus is largely on contacts per WTE, which has little meaning if the treatment value of the contact is unknown. Contacts will often be just ‘check ins’ particularly when services are ‘holding’ patients because they are risk-averse &/or have no organised themselves to deliver time-limited interventions.
This ‘holding’ common in the likes of a CMHT massively increases cost per case and demands more staff to meet the needs of new referrals.
Wards
Wards too have a similar issue. All mental health trusts are working to ensure purposeful admission in the first instance. You’d be surprised to note that at anytime 1 in 3 or more of inpatients are repeat admitters in the prior 12months, multiple admissions are common. This is containment not treatment.
Ward stays also become extended, adding further to the need for high cost beds. Facilitating early discharge demands close working between ward and community teams especially home treatment. This like 7 day working is still a challenge for most trusts to expedite flow.
Effective financial control
Budget planning is difficult, there is a reason why so many trusts struggle to balance the books, key reasons include:
- Forward visibility of funding and need to balance books at a system-level. How do you know a service development today is affordable next year?
- Quality will always trump money. A poor CQC report or service user tragedy will trigger a spend response. A senior manager is much more likely to be moved on for a quality over an economy failing, as the former has much more of a hold on the public.
- Finance and BI partnership at a service level is not strong. Even when there has been the investment in partners to guide the effective use of resource, this is undermined either because:
- the partners are working too remotely from the frontline…and have not built the relationships or understanding of services to challenge clinical and operational leads; or
- the underlying data structure and cost centre hierarchies to align workforce and activity is not in place to facilitate value for money insights
Is it any wonder that Finance Directors will look to reserves and unfilled vacancies to balance their books, whilst cost improvement programmes (CIPs) schemes, unloved by clinicians, go undelivered.
There is another way…
Don’t talk about the money
Get it right first time, good process is our friend. We must ensure service models are clear with a focus on removing from process and pathways non value-adding activity.
In a mental health environment this means service models that are:
- Time limited
- Co-produced around need (not what we can do)
- Joined up, so across different teams all can see:
- who knows the patient best;
- how their need is being met; &
- what to do in a crisis
And ensuring process improvement, such as applying Lean methodologies, are a core competency.
The drivers of efficiency are not hard to list, I call this my mental health ‘wheel of fortune’.
Wheel of fortune
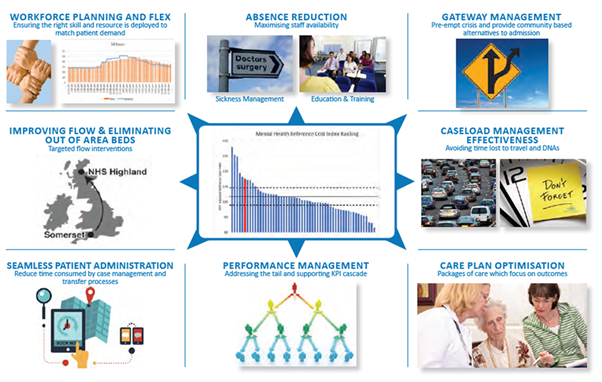
I have already touched on time lost to patient administration or poorly designed process; teams ‘holding’ service users with an absence of time limited intervention is a failure to care plan optimise. The ‘wheel’ additionally includes workforce planning and flex; performance management and absence reduction.
Conversations that focus on doing ‘wheel’ things better will energise clinicians. Money discussions can, however, suck the life out of a room. So our advice is leave CIP quantification to the finance partner to work up offline!
Back office
This leaves corporate areas, which need to lead by example. Just as front line services struggle to record the value they bring to service users, so too back office functions.
I led the NHSI sponsored national Financial Improvement Programme support when paired with Avon & Wiltshire Partnership pre-Covid. The executive team did not shy away from back office savings, sending a clear message by down-sizing and relocating HQ. Whilst importantly recognising the need to invest in the skills to support front line productivity improvement.
What if savings need to be realised at pace?
As any turnaround professional knows you have to grab the cheque book to buy time to reengineer operations. This can be uncomfortable as it requires a command-and-control management style.
Vacancy panels and imposing spend controls, with far more upward delegation is very demanding on an executive team. A necessary evil that no NHS organisation can preserve for long given the friction this generates with clinicians, who unlike a private business are not at risk of redundancy if financial rigour is not maintained.
Conclusion
Quality and economy go hand in hand. To get it right first time a mental health service user needs to experience timely purposeful time limited care.
There cannot be compromise on this, it is an operational model weakness if services are allowed to build a waiting list that then creates the further resource burden associated with waiting list management that reduces staff time available to treat.
Go back to the ‘wheel of fortune’ pick an operational improvement challenge, go from there to optimise value from your workforce and eliminate pressure on budgets.